Scientists at Sun Yat-sen University’s School of Biomedical Engineering have achieved a major breakthrough in bone regeneration by developing advanced tubular scaffolds using electrospun membranes. These innovative scaffolds are designed to mimic the natural structure of bone, providing an ideal environment for stem cells to promote the healing of critical skull defects, representing a significant advancement in tissue engineering and regenerative medicine.
Tackling Critical Bone Defects
Critical-sized bone defects have long posed challenges for medical professionals. Traditional treatments like autografts and allografts face limitations, such as donor scarcity, size mismatches, and potential immune rejection, making them less ideal for widespread use in bone repair. However, the emerging field of bone tissue engineering offers promising alternatives.
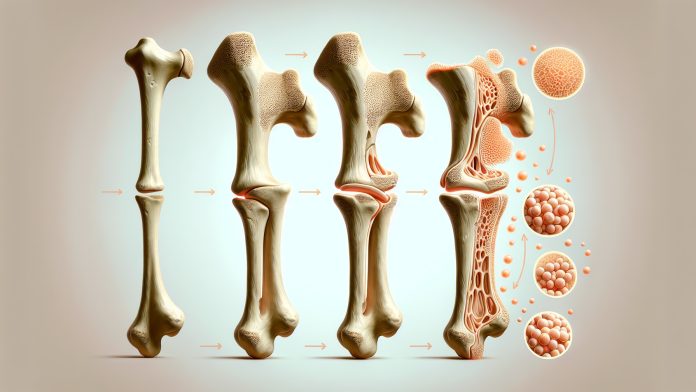
Adipose-derived stem cells (ADSCs), known for their strong osteogenic (bone-forming) properties, are increasingly recognized for their potential in bone regeneration. While injecting ADSCs directly into defect sites often leads to short survival times, combining them with scaffold materials has proven to improve cell retention and enhance bone regeneration. Researchers are now focused on creating scaffolds that closely resemble the natural bone structure using advanced technologies like electrospinning and 3D printing.
Innovative Tubular Scaffolds for Bone Regeneration
The team at Sun Yat-sen University developed multilayer composite nanofibrous membranes composed of polycaprolactone (PCL), poly(lactic-co-glycolic acid) (PLGA), and nano-hydroxyapatite (HAp). These materials, produced using electrospinning technology, are engineered to replicate bone’s structure. When formed into tubular scaffolds, they create an optimal environment for adipose-derived stem cells (rADSCs) to accelerate bone regeneration.
The scaffolds not only mimic the architecture of bone but also promote the proliferation and osteogenic differentiation of rADSCs, helping these stem cells transform into bone-forming cells more effectively. Laboratory and animal studies have shown remarkable success in promoting bone growth and healing with these scaffolds.
With a bilayer thickness ratio of 1:2 and an initial total thickness of 2.5 μm, these materials can spontaneously transform into 3D scaffolds under certain conditions, making them highly practical for medical applications.
The Future of Bone Regeneration
The success of these scaffolds points to a promising future for bone regeneration treatments. The research highlights the mechanisms by which these scaffolds, combined with growth factors like VEGF and BMP-2, stimulate bone formation. By integrating chemical signals with the physical properties of the scaffolds, this approach could revolutionize the treatment of bone defects.
Further research is needed to refine the design of these fibrous scaffolds and better understand how mesenchymal stem cells (MSCs) contribute to bone regeneration. However, the promising results so far suggest that these innovative scaffolds may soon find clinical applications, offering new hope for patients with critical bone defects.